Poor Egg Quality and Infertility: What You Need to Know
As a fertility specialist, one of the most heartbreaking issues I face is helping patients who are struggling with poor egg quality. It’s a topic that can stir a lot of emotions, as many women believe their dream of having children is slipping away. But, as I’ve learned throughout my career, poor egg quality is not the end of the road. In fact, it’s often just the beginning of a new path toward treatment and hope.
I remember one patient in particular, Emma, who came to see me after struggling with infertility for over two years. She was in her early 30s, had regular menstrual cycles, and her partner had a healthy sperm count. Despite this, they hadn’t been able to conceive. After running some tests, it became clear that her eggs weren’t up to the task—her ovarian reserve was low, and the quality of her eggs was deteriorating. It was a blow for Emma, but the journey we embarked on together ultimately led to a happy ending.

What Exactly Is Poor Egg Quality?
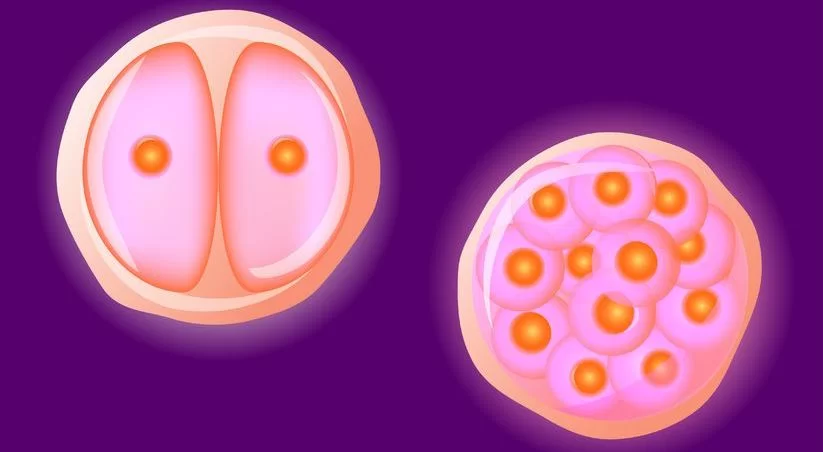
Before diving into treatment options, let’s first clarify what poor egg quality means. In simple terms, it refers to eggs that are not as healthy or viable as they should be. These eggs are less likely to fertilize or, if they do, they have a higher chance of not implanting or leading to miscarriage.
Egg quality is closely linked to age—as a woman gets older, the quality and quantity of her eggs naturally decline. However, other factors such as genetic issues, hormonal imbalances, lifestyle factors, or even environmental toxins can also contribute to poor egg quality.
Dr. Rachel Green, a leading reproductive endocrinologist, once told me, “The quality of a woman’s eggs is a critical factor in her ability to conceive, but it’s not always about the quantity. Even women with a good number of eggs can face challenges if the eggs themselves are not up to par.”

The Causes of Poor Egg Quality
In many cases, poor egg quality is linked to age, but there are other underlying factors that can contribute as well. Some of the most common causes include:
- Age: As women age, the number of eggs decreases, and the remaining eggs are more likely to have chromosomal abnormalities. This is why women over 35 often experience a decline in fertility.
- Genetics: Certain genetic conditions can impact egg quality. For example, women with Turner syndrome or Fragile X syndrome may have issues with egg development or function.
- Lifestyle Factors: Smoking, excessive alcohol consumption, poor diet, and lack of exercise can all contribute to poorer egg quality. I’ve seen it firsthand—patients who make healthier lifestyle changes often see improvements in their egg quality.
- Hormonal Imbalances: Conditions like Polycystic Ovary Syndrome (PCOS) or premature ovarian insufficiency (POI) can affect the hormonal signals necessary for healthy egg production.
- Environmental Toxins: Exposure to environmental toxins, such as pesticides, chemicals, and even plastics, can interfere with egg quality. This is a growing area of concern in fertility medicine.

Diagnosing Poor Egg Quality
Diagnosing poor egg quality is not always straightforward, but there are a few key tests we rely on to assess a woman’s egg reserve and quality. These include:
- AMH (Anti-Müllerian Hormone) Test: This blood test measures the hormone produced by follicles in the ovaries. A low AMH level can indicate a lower ovarian reserve and possibly poorer egg quality.
- FSH (Follicle-Stimulating Hormone) Test: Elevated FSH levels on day 3 of the menstrual cycle can suggest that the ovaries are working harder to produce eggs, often a sign of diminished egg quality.
- Ultrasound: A transvaginal ultrasound can show the number and size of follicles in the ovaries, giving insight into the health of the eggs.
- Ovarian Biopsy: In rare cases, an ovarian biopsy may be performed to assess the quality of the eggs directly.
While these tests help identify the state of a woman’s ovarian reserve, they don’t always tell the whole story. Egg quality, unlike quantity, can’t be directly measured by blood tests alone.
The Emotional Toll of Poor Egg Quality
One of the hardest parts of dealing with poor egg quality is the emotional impact it has on women. It’s not just about the science; it’s about a dream—often a lifelong dream—that is now at risk. I’ve seen patients go through waves of frustration, guilt, and even shame, despite the fact that poor egg quality is rarely anyone’s fault.
I remember a patient named Megan, who was in her early 40s when she came to see me. She had tried for years to conceive with her partner, but after a series of failed IVF cycles, she was devastated to learn that her eggs had significant chromosomal abnormalities. Megan’s world was rocked. She felt that she had failed, that her body was betraying her.
But after discussing her options, Megan and I decided to try egg donor IVF—a path that ultimately led to her successful pregnancy. “I never thought this would be my story,” she said to me during one of our follow-up appointments. “But I’m finally pregnant, and I couldn’t be more thankful.”
Treatment Options for Poor Egg Quality
While poor egg quality can feel like a dead end, there are several options available for couples dealing with infertility due to this issue. The right path will depend on individual circumstances, but here are some of the most effective treatments:
- Lifestyle Changes: Improving diet, exercise, and reducing alcohol and smoking can sometimes improve egg quality. I’ve had patients see marked improvements after making these changes.
- Hormonal Support: For women with PCOS or hormonal imbalances, medications like Clomid or gonadotropins can stimulate the ovaries to produce better quality eggs.
- Egg Donor IVF: In cases of significantly poor egg quality, egg donation may be the best option. This allows a woman to carry a pregnancy using a donor egg, bypassing the issue of poor egg quality.
- Embryo Screening: For women who produce eggs that are not of optimal quality, preimplantation genetic testing (PGT) can be used during IVF to screen embryos for chromosomal abnormalities before implantation. This can improve the chances of a successful pregnancy.
- Stem Cell Therapy: Though still experimental, stem cell therapy is being studied as a potential treatment for poor egg quality by regenerating or rejuvenating eggs.
Dr. Emily Rivera, a leading expert in fertility treatment, once told me, “While we can’t turn back the biological clock, there are advanced treatments that allow women to have a healthy pregnancy, even with poor egg quality.”
Moving Forward with Hope
The journey with poor egg quality can feel long and uncertain, but it’s important to remember that there is hope. Whether it’s through lifestyle changes, advanced fertility treatments, or the use of egg donation, women who face poor egg quality are not without options. It’s a challenging path, but with the right care, support, and determination, many women and couples can go on to have the families they’ve always dreamed of.
I’ve seen countless patients, like Emma and Megan, overcome the challenges of poor egg quality and achieve their dream of becoming parents. And that’s what keeps me going every day. Fertility treatment is never easy, but the reward of seeing a family grow is worth every step of the journey.



