Low Sperm Count and Infertility: A Fertility Specialist’s Journey
As a fertility specialist, I’ve had the opportunity to work with countless individuals and couples struggling with infertility. When it comes to male infertility, one of the most common causes I see is low sperm count. Often, it’s a topic that men are uncomfortable discussing. It’s not always easy for them to face the reality that they might be the cause of the fertility struggles in their relationship, but it’s a problem that can be addressed with the right approach.

Understanding Low Sperm Count
Low sperm count, or oligospermia, is when a man has fewer sperm in his semen than normal. For a semen sample to be considered normal, it typically needs to have at least 15 million sperm per milliliter of semen. Anything less than that could potentially cause difficulty in achieving pregnancy. But sperm count is only part of the equation. Sperm quality—how well the sperm move (motility) and their shape (morphology)—is just as important. A low sperm count doesn’t automatically mean a man cannot father a child, but it does increase the challenges.
I’ll never forget a patient named Mark, who came to me with his wife, Linda. They had been trying to conceive for over two years without success, and both were at a loss for what was happening. Mark had a normal sex drive, and Linda’s cycles were regular, but after a few tests, we discovered that Mark’s sperm count was extremely low—well below the threshold for natural conception.
Dr. Nathan Hughes, a renowned urologist who specializes in male fertility, once told me, “Sperm count is just the start of the conversation. It’s the combination of quantity, quality, and other factors that determines fertility.” That advice has stuck with me over the years, and it’s something I always remind my patients. A low sperm count doesn’t always mean the end of the road for a couple. There are solutions, but it requires a holistic and personalized approach.

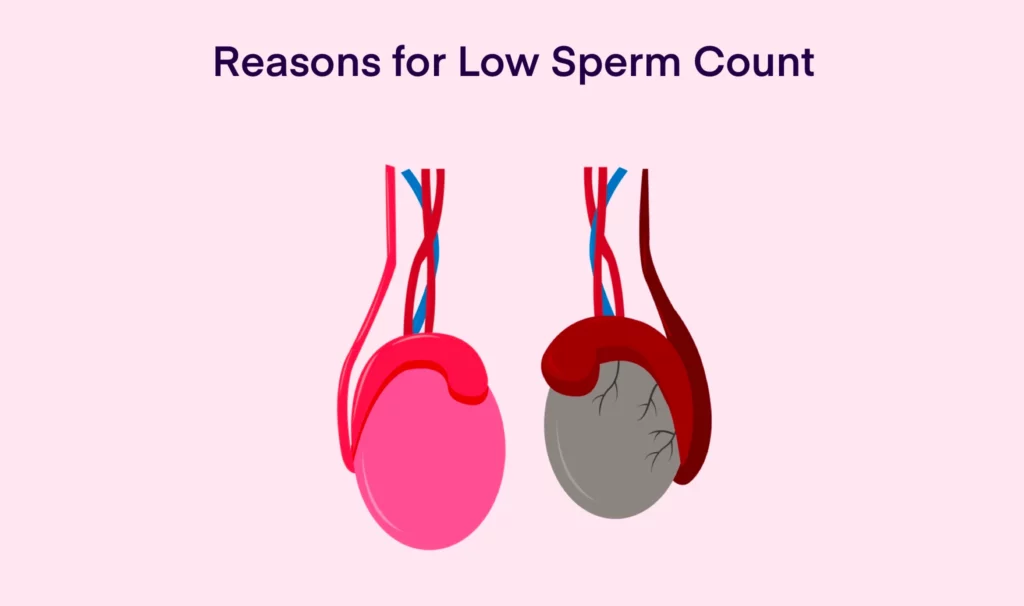
The Causes of Low Sperm Count
The causes of low sperm count can vary. In many cases, the problem is linked to lifestyle factors such as smoking, excessive alcohol consumption, poor diet, or lack of exercise. Environmental factors like exposure to heat, toxins, or radiation can also play a role. Other medical conditions, such as varicocele (a swelling of veins in the scrotum), infections, or hormonal imbalances, can affect sperm production. In some cases, no clear cause is found, and the problem is simply labeled as idiopathic, meaning the cause is unknown.
When Mark first came to see me, we ran a series of tests to check for potential causes. It turned out that he had a varicocele, which can increase the temperature of the testes and disrupt sperm production. This was a big piece of the puzzle. Mark was referred for surgery to correct the varicocele, and after a few months, his sperm count increased significantly.
But even after surgery, we still had to tackle the emotional and psychological toll infertility had taken on them. Linda, especially, felt a sense of guilt—like it was somehow her fault. This is something I see frequently in my practice. Infertility affects both partners, but it’s often the woman who bears the brunt of the emotional burden.

Treatment Options for Low Sperm Count
Once we determined the cause of Mark’s low sperm count, we explored treatment options. For many men, lifestyle changes can have a significant impact. I often recommend improving diet, exercising regularly, and reducing alcohol and tobacco use. For some men, vitamins like Vitamin C and zinc may help improve sperm health. But it’s not always as simple as making lifestyle changes.
For men with severe oligospermia or those who don’t respond to medical treatments, assisted reproductive technologies (ART) are often the next step. In in vitro fertilization (IVF), sperm are directly injected into an egg through a process called intracytoplasmic sperm injection (ICSI). This allows us to bypass the sperm count issue altogether, increasing the chances of successful fertilization.
Another option is sperm retrieval surgery, which is used for men with very low sperm counts or who are producing no sperm at all. During this procedure, sperm can be extracted directly from the testicles or epididymis and then used in ART procedures.
In Mark’s case, after his varicocele surgery, we decided to try ICSI as a backup plan. The procedure was a success, and after just one cycle of IVF, Linda became pregnant with twins.
Dr. Lisa Monroe, a leading fertility expert, once said, “In male infertility, we often focus too much on the sperm count itself, and not enough on the solutions available. There’s always a path forward.” That’s something I take to heart when working with my patients. While a low sperm count can feel like a major roadblock, it’s rarely the end of the journey.
The Emotional Impact of Low Sperm Count
While the medical side of infertility can be overwhelming, I’ve come to realize that the emotional challenges men face are just as significant. Many men feel embarrassed, ashamed, or frustrated when they learn that they are the ones with the fertility issue. It can be difficult to navigate the impact on their relationship, as the pressure mounts to “fix” the problem.
Mark and Linda’s case was a reminder of just how much infertility can affect a couple’s mental and emotional health. Mark was initially reluctant to talk about the issue, but after a few sessions, he opened up about how the diagnosis had made him feel inadequate. It was clear that the emotional toll of infertility was as challenging as the physical aspects for them.
I often tell my patients, “Infertility is a couple’s journey, not just an individual’s struggle.” That’s why it’s so important to address the emotional side of the process—whether through therapy, support groups, or simply having open and honest conversations with your partner. I encourage men to talk about their feelings and not bottle up their emotions, because infertility can feel like an invisible weight on both partners.
The Future of Male Infertility Treatments
The good news is that the field of male infertility is advancing rapidly. New technologies, better diagnostic tools, and improved treatments are giving couples more hope than ever before. From sperm preservation for men undergoing cancer treatment to advancements in ICSI and genetic screening, the possibilities for men facing low sperm count are expanding.
The key takeaway here is that low sperm count doesn’t have to be a dead end. Whether it’s through lifestyle changes, surgery, or ART, there are many ways to increase the chances of a successful pregnancy. The path to parenthood might be longer or more complicated, but it’s still possible.
So to any man reading this who has been diagnosed with low sperm count: don’t lose hope. With the right medical care and emotional support, you and your partner can still achieve your dream of becoming parents.



